What to expect from each investigation
We offer an extensive range of prenatal diagnostics for the examination of your baby and for your wellbeing. With our expertise, i.e. specialist qualifications in prenatal diagnostics, state-of-the-art high-resolution ultrasound and colour Doppler imaging equipment including 3D/4D, we are especially equipped for this purpose.
In order to be able to offer you the maximum security of the examination, the desired examination should take place at an optimal time. If, for example, the examination is possible from the 11+0th week of pregnancy (SSW), then this means that you must be at least in the 12th week of pregnancy.
| Investigation method | Optimal time during pregnancy | Aim |
|---|---|---|
| NIPT (Non-Invasive Prenatal Testing) | From 11+0 week of pregnancy | Risk assessment for a trisomy 21 |
| Chrionic villus sampling | From 11+0 week of pregnancy | Chromosomal examination, exclusion of trisomy 21 |
| Early malformation screening/early fetal echocardiography | 12+0 – 13+6 week of pregnancy | Early exclusion or detection of malformations and developmental disorders |
| First trimester screening |
12+0 – 13+6 week of pregnancy | Risk assessment for a trisomy 21 |
| Pre-Eclampsia screening | 12+0 – 13+6 week of pregnancy | Risk assessment for pre-eclampsia |
| Amniotic fluid sampling | From 16+0 week of pregnancy | Chromosomal examination, exclusion of trisomy 21 |
| Umbilical cord blood sampling | From 18+0 week of pregnancy | Chromosomal examination, exclusion of trisomy 21 |
| High resolution ultrasound diagnostics/fetal Echocardiography | 20+0 – 21+6 week of pregnancy | Exclusion or detection of malformations and developmental disorders |
From 11+0 weeks of pregnancy
Deviations from the normal number of chromosomes (numerical aberrations) represent one of the most common causes of congenital disorders of the child. The most common disorder is trisomy 21, where there is an extra copy of chromosome 21 (3 instead of 2) in the cell nucleus. This leads to Down's syndrome. A trisomy of chromosomes 13 and 18 is rarer.
The probability of the birth of a baby with a chromosomal change depends especially on the age of the mother. Whilst the risk of having a child with Down’s syndrome is 1: 1500 for a 20 year old mother, it rises to 1: 100 at birth for a 40-year-old mother.
Prenatal invasive techniques for the analysis of the chromosome set of the unborn child are available. They are called amniocentesis and chorionic villus sampling. Whilst both techniques can very reliably identify chromosomal alterations, the respective techniques are associated with a procedure-related miscarriage risk, which is reported to be about 0.3% -0.6%.
Non-invasive methods for risk assessment, such as first-trimester screening, allow an individual risk assessment based on biochemical blood tests and ultrasound markers. The chance of chromosomal abnormalities in the child can thereby be individually assessed. However, the procedures do not allow a direct diagnostic statement about the baby’s chromosomes to be made.
Since 2012, molecular genetic tests have been available that allow which allow the most common chromosomal abnormalities to be diagnosed with high certainty non-invasively using the mother's blood. The methods are collectively referred to as non-invasive prenatal testing or NIPT. The basic principle is that small fragments of the baby’s genetic material (DNA) are present in the mother's blood in the cell-free blood plasma, so-called cell-free fetal DNA (cffDNA). The baby’s cell-free DNA makes up about 10% of the total cell-free DNA. These DNA fragments are derived from the placenta. This fetal cell-free DNA can be analysed using the latest molecular biological techniques to determine whether more DNA appears from one chromosome that would be expected. This procedure can diagnose or exclude trisomy 13, 18 or 21 with a very high certainty. Analysis of the number of sex chromosomes (e.g. diagnosis of Turner syndrome) and the reliable determination of the sex of the child are also possible.
The diagnostic reliability is high; the detection rate (probability of detecting an existing fault) is about 99% for trisomy 21. With an incidence of 0.08%, false positives (a chromosomal disorder is indicated that is truly not present) occur only rarely, therefore unusual results should be thoroughly reviewed with invasive procedures.
NIPT is especially offered to women with an increased with of one of the named chromosomal abnormalities, e.g., after an abnormal first trimester screening.
Please note:
The techniques are not currently listed in the service catalogue of the health insurance companies (Krankenkassen) as part of prenatal care. We only perform NIPT after specific malformation screening and a detailed consultation. This additional diagnostic test can also be performed if you agree to cover the cost yourself.
From 11+0 weeks of pregnancy
Since the placenta (known as the chorion in early pregnancy) originates from the fertilised egg cell, cells can be removed for analysis of the baby’s chromosomes.
The test is useful when a chromosome analysis is necessary very early in the pregnancy, where there are noticeable problems with the embryo in the ultrasound image, for high-risk patients as part of first-trimester screening, for hereditary disorders or metabolic disease in the family or if you have an expressive request after an early diagnosis. This method does not give any information about cleft malformations in the spine (neural tube defects).
12+0 – 13+6 weeks of pregnancy
During this early stage of the pregnancy, we perform early malformation screening if the scan conditions are good and can then already rule out 40-50% of all malformations. However, external circumstances such as a think maternal abdominal wall or unfavorable positioning of the baby limit the investigation, despite the use of high-resolution ultrasound equipment. The optimal time for this diagnosis is between 12 + 0 and 13 + 6 weeks.
11+1 – 13+6 weeks of pregnancy
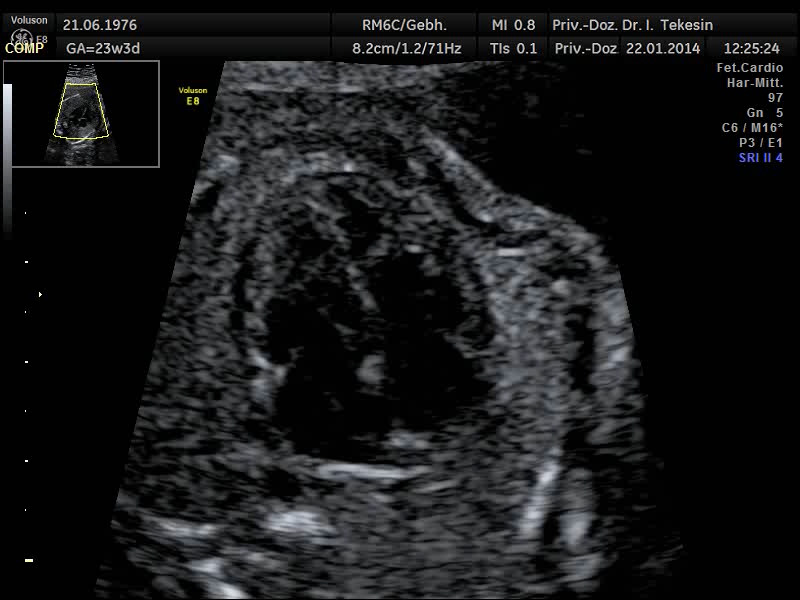
With high-resolution ultrasound equipment and appropriate training of the doctor, the baby’s heart can be assessed as part of an early fetal echocardiography at an earlier stage, i.e. between the 12th and 15th week of pregnancy. If the heart appears normal during these weeks of pregnancy, up to 65% of heart defects can be excluded. A normal early fetal echocardiography should always be followed by a scan of the baby’s heart in the 20th to 22nd weeks of pregnancy (some heart defects can develop later during pregnancy).
12+0 – 13+6 weeks of pregnancy
By measuring the fetal nuchal translucency, a risk assessment in relation to age-related chromosomal disorders such as trisomy 21, trisomy 18 and trisomy 13 can be carried out from the 11th until the end of the 13th week of pregnancy. During this time, we often find water retention under the skin on the neck (called nuchal translucency or NT). In addition to the NT measurement, we examine other ultrasound markers such as the nasal bone, the tricuspid valve blood flow and the ductus venosus. If the NT is widened, for example, the probability of the baby having a disorder increases. The measurement requires an ultrasound device with good resolution and an experienced examiner. The validity of the ultrasound screening can be increased with an additional maternal blood test (PAPP-A and free ß-HCG), a so-called “combined test”.
12+0 – 13+6 weeks of pregnancy
Some women may develop serious complications during the course of a pregnancy. Recent studies have shown that indicators of possible later complications (especially high-blood pressure disorders) can already be found in the first trimester of pregnancy.
Preeclampsia (formerly "pregnancy intoxication, late gestosis”) is one of the most common complications during pregnancy. In 2% of all pregnant women, this disease occurs before the 32th week of pregnancy. This early pre-eclampsia is also often combined with intrauterine growth retardation (IUGR) of the baby. Pre-eclampsia (PE) can therefore be very dangerous for mother and child.
Although signs of illness only appear after the 20th week, the real cause, impaired implantation and development of the placenta, develops in the first trimester of pregnancy. Therefore, any risk of pre-eclampsia should be detected as early as possible, so that prophylaxis can be started as early as possible and the pregnancy can be closely monitored.
In addition to PAPP-A measured in the first-trimester screening, there is another new parameter in the blood of pregnant women, placental growth factor (PlGF). In pre-eclampsia and in the case of later IUGR, this parameter is found to be lower in early pregnancy, i.e. before the complications occur, and is therefore suitable for screening. Both parameters are made in the placenta and low concentrations in the maternal blood indicate complications (preeclampsia / IUGR) in later pregnancy.
At the request of the patient or for certain indications, an individual risk for the development of a blood pressure disorder (pre-eclampsia) later in the pregnancy can be calculated in a differentiated ultrasound scan in the 12th to 14th week of pregnancy (ideally as part of first trimester screening). Besides the two biochemical parameters PAPP-A and PlGF, the medical history and clinical data of the pregnant mother (such as age, weight, arterial blood pressure) and the flow rate of blood in the uterine artery (Doppler sonography) are included in the calculation. The detection rate for the occurrence of pre-eclampsia before 34 weeks, considering the above data, is about 95 percent. This applies for a threshold of risk of 1: 200 and a false-positive rate of 11 percent.
If an increased risk is found, prophylaxis with low-dose aspirin (100 mg per day) should be started straight away. The occurrence of pre-eclampsia can thereby be significantly reduced in women with an increased risk and also serious illness can be delayed until a later stage of pregnancy.
Please note:
Pre-eclampsia screening is not part of the regular check-ups during pregnancy. The cost of counselling, ultrasound and laboratory tests are not covered by the statutory health insurance companies (Krankenkassen).
From 16+0 weeks of pregnancy
Amniotic fluid testing is not included in the normal pregnancy check-ups and requires detailed counselling. Many congenital defects can be detected with this test, e.g. chromosomal abnormalities, neural tube defects and hereditary illnesses, provided that they are detectable with today’s technology and that the other family members have been tested. We only perform amniocentesis after at least 15 completed weeks of pregnancy in order to reduce complications that an earlier test may cause.
From 18+0 weeks of pregnancy
Umbilical cord blood sampling is only performed in certain situations, for example where there is blood group incompatibility, infection during pregnancy, fetal anaemia, where there is suspicion of metabolic disease in the baby and where there are noticeable problems seen on ultrasound in the later weeks of pregnancy. About 2mls of the baby’s blood are removed. This procedure can only be carried out after 18 weeks of pregnancy. In certain circumstances, medication or blood products can be fed into the baby’s circulation (intrauterine transfusion).
20+0 – 21+6 weeks of pregnancy
Ultrasound examination is an imaging technique which, according to current knowledge, does not cause any damage to mother or child, even after repeated use.
We offer high-resolution ultrasound diagnostics at an optimal time of between the 20th and 22nd week of pregnancy. This investigation is considerably more extensive than the ultrasound scan which is specified in the maternity guidelines for this stage of pregnancy. Alongside the need for special equipment, the doctor performing the scan also requires considerable experience.
Under good ultrasound conditions, the scan usually takes between 30 and 45 minutes. The position of the baby and the thickness of the mother’s abdominal wall play a decisive role in this. We examine all the visible organs and features of the unborn baby: the baby’s age-appropriate growth, the amount of amniotic fluid, the appearance and function of all visible organs and the location and appearance of the placenta.
The detailed ultrasound scan may also detect features that increase the statistical risk for the presence of Down's syndrome in some unborn babies. These abnormalities are not malformations and they do not have any adverse effects on the organs affected. If we discover one or more of these so-called "markers" during the investigation, we can perform a Down’s syndrome risk assessment whilst taking your age into consideration.
Limits of ultrasound diagnostics
With the help of ultrasound diagnostics, about 90% of malformations or disorders of the child can be recognized and, above all, excluded. On the other hand, it must be explicitly pointed out that even with modern equipment, the utmost care and the doctor’s extensive experience, not all malformations or diseases can be detected.
The oversight or misjudgement of a malformation may also result from the fact that in certain circumstances (e.g. a fat abdominal wall, low amniotic fluid volume, positioning of the baby), the scan conditions are made difficult. Findings recognisable using ultrasound cannot always be clearly classified in their significance.
It is possible that minor defects are not recognized, such as for example, a hole in the dividing wall between the heart chambers, or finger or toe deformities
It should be noted that every pregnancy has a so-called basis risk of 2 - 4% for malformations and diseases in the child, about 1% of which are serious malformations. This basis risk is increased in insulin-dependent pregnancy diabetes in the mother or in multiple pregnancies. The exclusion of chromosomal abnormalities as an alternative to invasive diagnostics (amniotic fluid or umbilical cord blood) is possible in principle by the detection of characteristic, but not mandatory signs of chromosomal abnormalities. The absence of these typical findings can reduce the risk of having a child with chromosomal abnormalities (e.g. Down’s syndrome), but not rule it out.
This examination is much more extensive than the ultrasound examination provided for in the maternity guidelines at that time. In addition to special equipment, it also requires a great deal of experience on the part of the examiner.
Under good ultrasound conditions, this examination normally takes about 20 to 30 minutes. The position of the child and the thickness of the mother's abdominal wall play a decisive role. In doing so, we look at all presentable organs and characteristics of the unborn child: the age-appropriate fetal growth, the amount of amniotic fluid, the appearance and function of all visible organs and the position and appearance of the placenta.
During the detailed ultrasound examination, some unborn children may also show features that increase the statistical risk of Down syndrome. These abnormalities are not malformations, nor do they cause any impairment of the affected organs. If we discover one or more such so-called "markers" during the examination, we can carry out a risk assessment with regard to Down syndrome, taking your age into account.
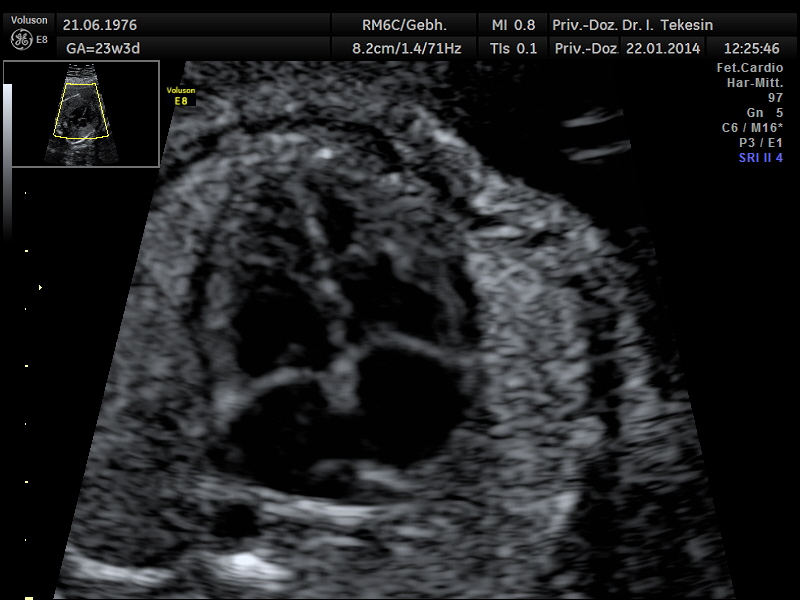
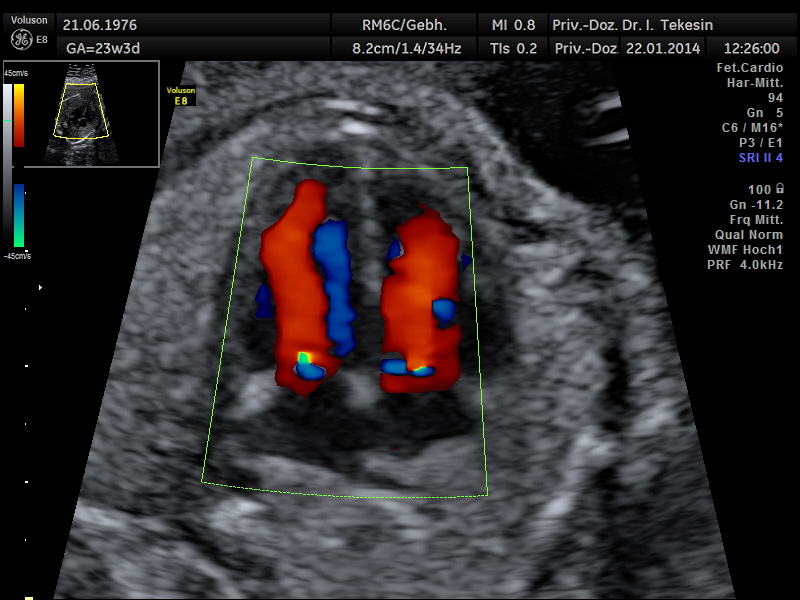
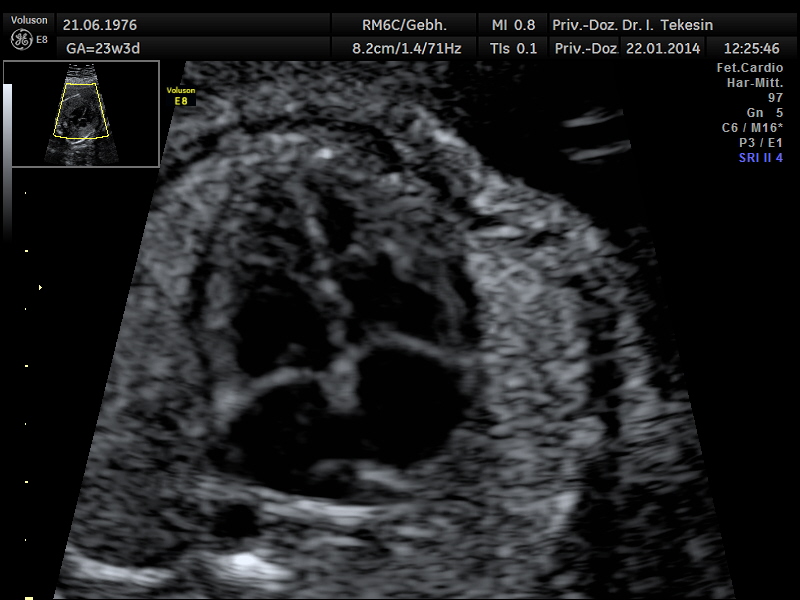
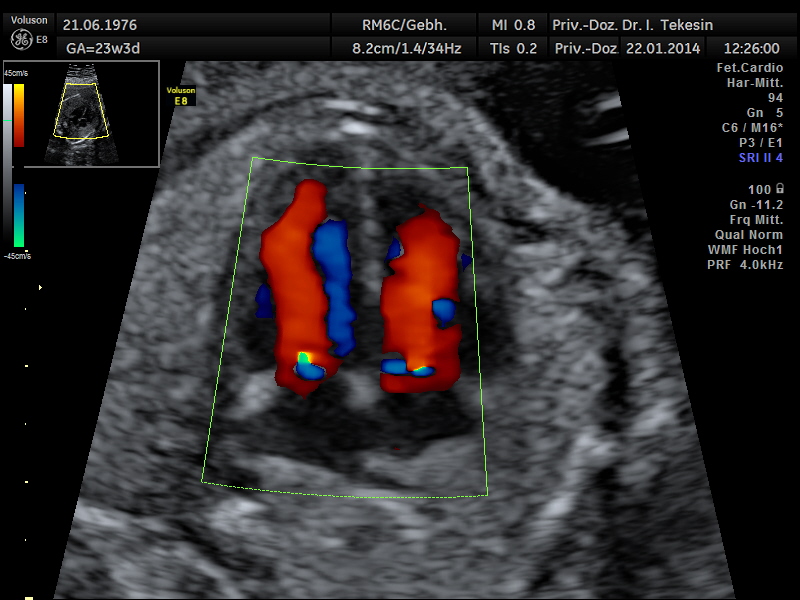
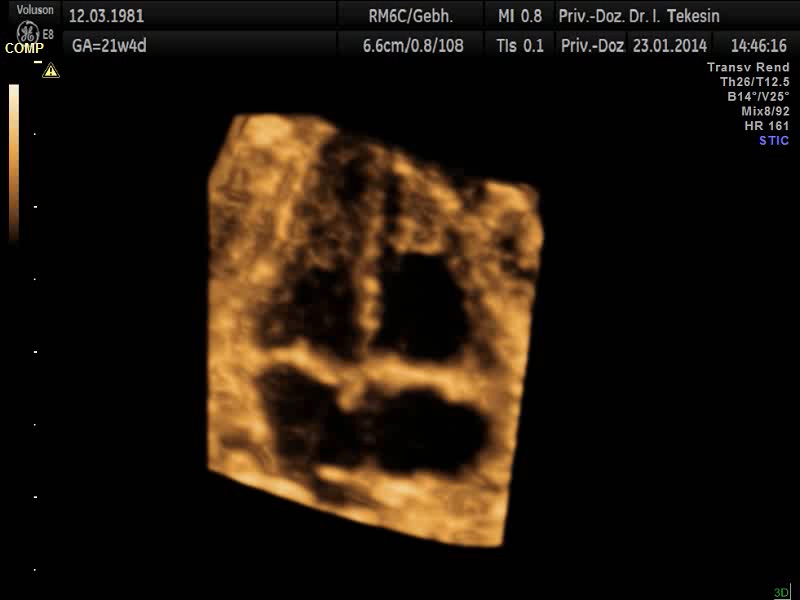
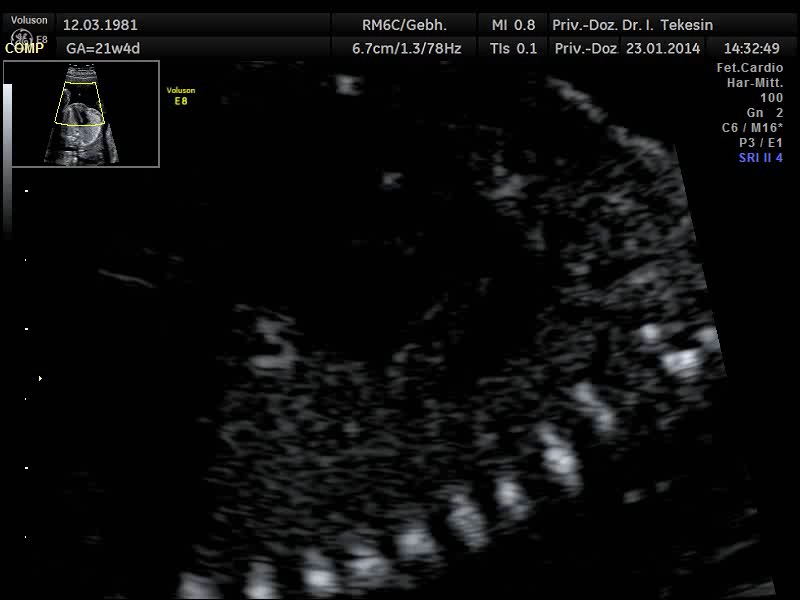
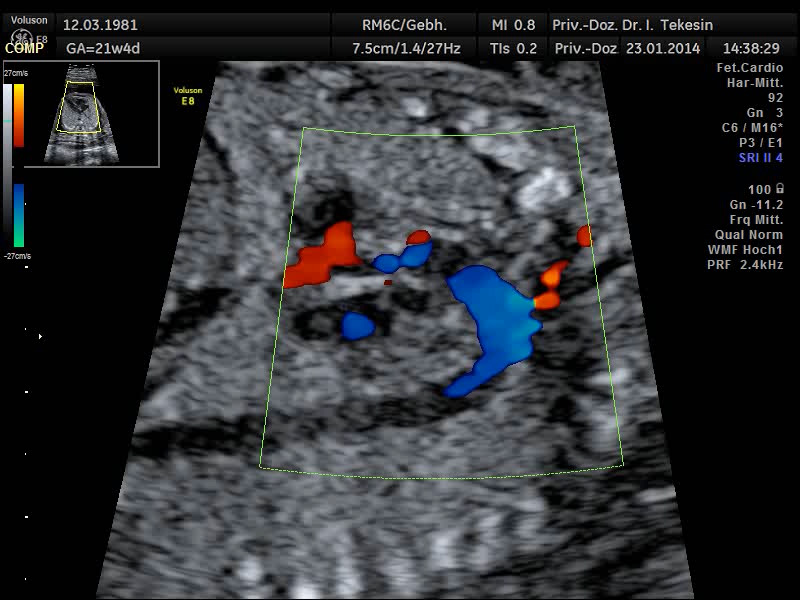
Another component of advanced ultrasound diagnostics is the assessment of the baby’s heart and large blood vessels, fetal echocardiography. The position, size and symmetry of the heart, anatomy of the heart structures, function of the heart valves, heart rate and position of the large vessels are examined. Using colour-coded Doppler sonography of the heart, further details can be examined: the function of the heart chambers, the heart septum, blood flow through the heart and blood flow through the large vessels.
The aim of the ultrasound examination of the fetal heart is to exclude congenital heart disease as far as possible. The prerequisite for this is the doctor’s specialist education and experience together with the high quality of the ultrasound device.
About 7,000 children are born alive with structural heart defects in Germany every year. With an incidence of 1:100, heart malformations are amongst the most common congenital malformations. Surgery is required in about half of heart malformations based on the severity of the malformation. By improving prenatal diagnosis, the recognition rate of fetal cardiac abnormalities can be significantly increased, enabling the young patients to have a better start in life with immediate specialist treatment.
Thanks to the increasing improvement of the equipment and the training of specialist doctors, the majority of cardiac malformations can already be detected or ruled out between the 13th and 14th week of pregnancy.
The final assessment of the heart, its function and blood flows is performed between the 19th and 21st week of pregnancy and should usually by completed by the 22nd/23rd week. At a later stage in the pregnancy, the scan is often adversely affected by unfavourable positioning of the child, as well as by the poor ultrasound transmission through the ribs.
Most congenital heart diseases (about 83%) can be recognized using fetal echocardiography. However, there are heart defects which are not yet visible (or are difficult to visualise) in the 20th week of pregnancy. These include narrowing of the heart valves, the consequences of which are visible only later. Even a small "hole" in the dividing wall between the heart chambers is not always detectable.
Most congenital heart defects can be operated on very well today. The success rate of the treatment increases demonstrably if it has been discovered before birth.
If a fetal heart defect is found or suspected, specific counselling takes place involving paediatric cardiologists. We discuss with you where and under what conditions the birth should take place and the treatment plan after the birth.
Even the blood circulation in the umbilical cord and the uterine vessels can be visualised using Doppler ultrasound. This is an additional examination as part of the high-resolution ultrasound scan and allows the assessment of blow flow in the baby’s and mother’s vessels using a special technique. The blood flow is presented in both colour and sound. The sounds that you hear during the Doppler scan originate from technical effects (the Doppler effect) which neither the doctor, the parents nor the unborn child can hear.
By visualising the blood flow patterns in the maternal vessels (the right and left uterine arteries) between the 20th-25th week of pregnancy, fetuses with a risk of a later insufficient blood supply (placental insufficiency) may be detected and thus optimally monitored during the course of pregnancy. An increased risk of developing pre-eclampsia (maternal high blood pressure and protein in the urine) can also be found.
The assessment of blood flow in the infantile vessels (umbilical artery [A. umbilicalis], A. cerebri media and ductus venosus) allows a statement on the blood supply to the unborn child to be made. The Doppler examination can be carried out at different times during pregnancy.
If in the Doppler sonography reveals a suspected deficient blow flow to the child or a pre-eclampsia, preventive measures can be initiated in accordance with the current high-risk pregnancy precautionary measures.
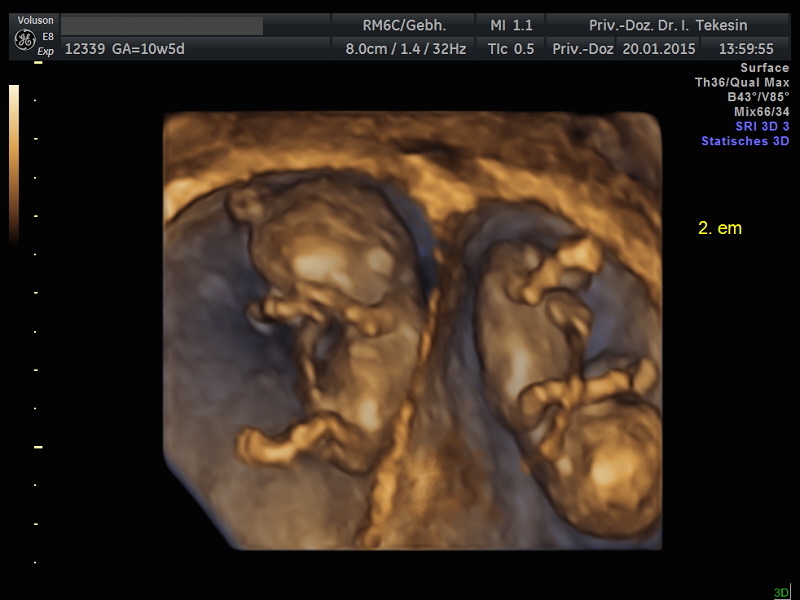
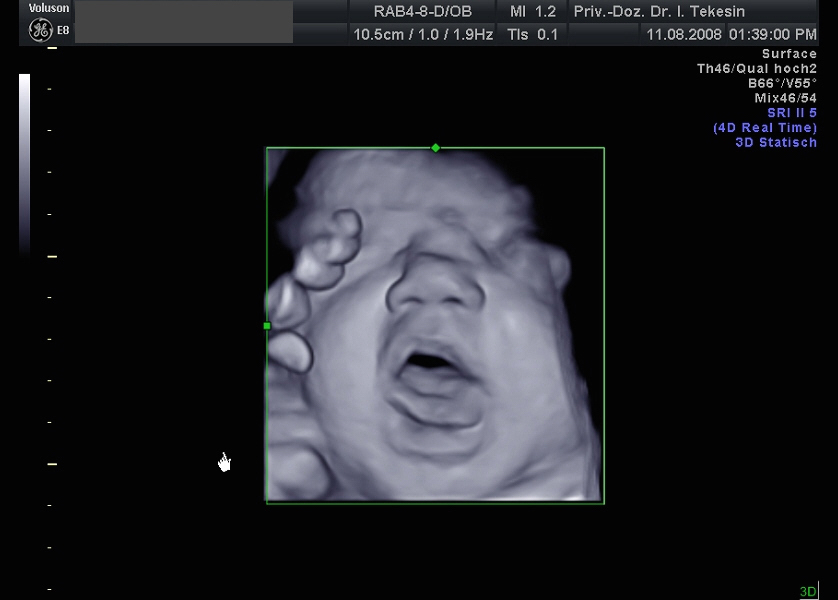
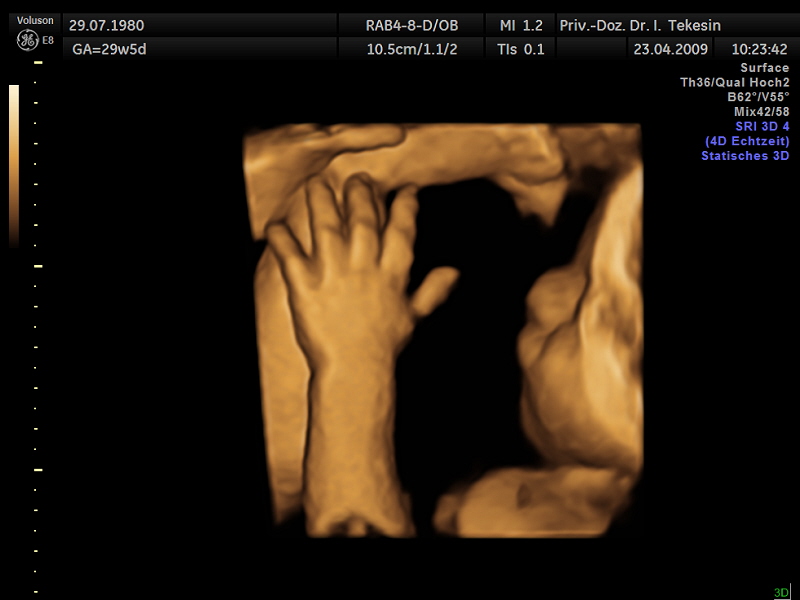
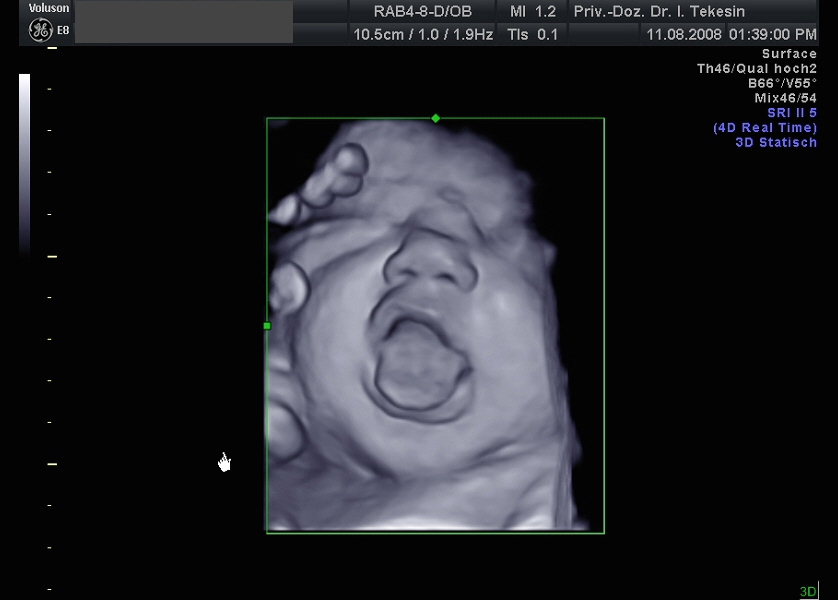
More and more parents-to-be are interested in the fascinating images that this technique provides. The structural, 3-dimensional portrayal of the face and other parts of the body is achieved by fast processing of special image reconstructions. Individual internal organs and “vascular trees” can also be visualised from all sides. Many thin section planes (2D) are merged into a three-dimensional image in the ultrasound device’s computer. A 4D ultrasound is a 3D ultrasound scan under real-time conditions. Instead of displaying only static images, a 4D ultrasound detects the movements of the child, which is why it is also called "live 3D ultrasound".
This approach enables highly realistic images, in which even gestures and facial expressions of the child can be recorded in moving sequences. Just like the normal ultrasound scan, this scan can be carried during the entire pregnancy. If you would like to see the unborn baby completely, the best time for this is the 12th to 16th week of pregnancy; the time between the 28th and 33rd week of pregnancy is particularly suitable for precise visualisation of individual body parts.
This modern method is primarily a supplementary measure in special cases where there are questions regarding the heart, brain or skeleton and especially in cases where there is a suspected fetal anomaly.
Please note:
The 3D / 4D methods are not currently listed in the service catalogue of the health insurance companies (Krankenkassen) as part of prenatal care. We only perform this scan if there is a previous malformation diagnosis. This additional scan can also be performed if you agree to cover the cost yourself.